Chronic kidney disease in cats (often shortened to CKD in cats) is one of the most common health issues seen in middle-aged and senior cats. Kidney problems develop slowly, which means many early warning signs can be subtle. Early recognition gives cats a better quality of life, helps slow the progression of CKD, and allows vets to rule out other conditions like kidney stones in cats or urinary blockages.
Without further due here are the 10 early signs veterinarians most want cat owners to notice:
1. Increased Thirst (Polydipsia)
One of the earliest and most classic signs of chronic kidney disease in cats is drinking more water than usual. You may see your cat visiting the water bowl more often or drinking from unusual places like the sink or bathtub.
2. Frequent Urination
Kidneys lose their ability to concentrate urine in the early stages of CKD in cats, which leads to larger volumes of pale urine. Cats may fill the litter box more quickly or urinate outside the box if they can’t make it in time.
3. Weight Loss
As chronic kidney disease in cats progresses, the body struggles to maintain muscle mass. Even if your cat eats normally, you may notice gradual weight loss. Veterinarians consider this one of the most important warning signs.
4. Reduced Appetite
Cats with kidney disease often eat less because of nausea or changes in metabolism. A decreasing appetite over weeks not just a day or two should prompt a vet check.
5. Vomiting or Nausea
Another common symptom in chronic kidney disease in cats is digestive upset. Occasional vomiting may be easy to overlook, but repeated episodes can be related to kidney stress.
6. Bad Breath (Uremic Odor)
Chronic kidney disease in cats may also cause a distinctive ammonia-like smell on their breath. This isn’t a dental issue; it’s a sign of waste products building up in the bloodstream.
7. Lethargy and Less Interest in Play
A cat with early kidney disease may seem “slowed down,” sleep more, or lose enthusiasm for normal activities. Because this symptom is vague, many owners mistake it for normal aging.
8. Poor Coat Quality
Chronic kidney disease in cats may cause the cat to groom less or have dull, dry fur. Muscle loss and dehydration make their coat look scruffy or unkempt.
9. Dehydration
Even though many cats drink more when their kidneys fail, they can still end up dehydrated. Signs of dehydration in chronic kidney disease in cats include sunken eyes, dry gums, and overall low energy.
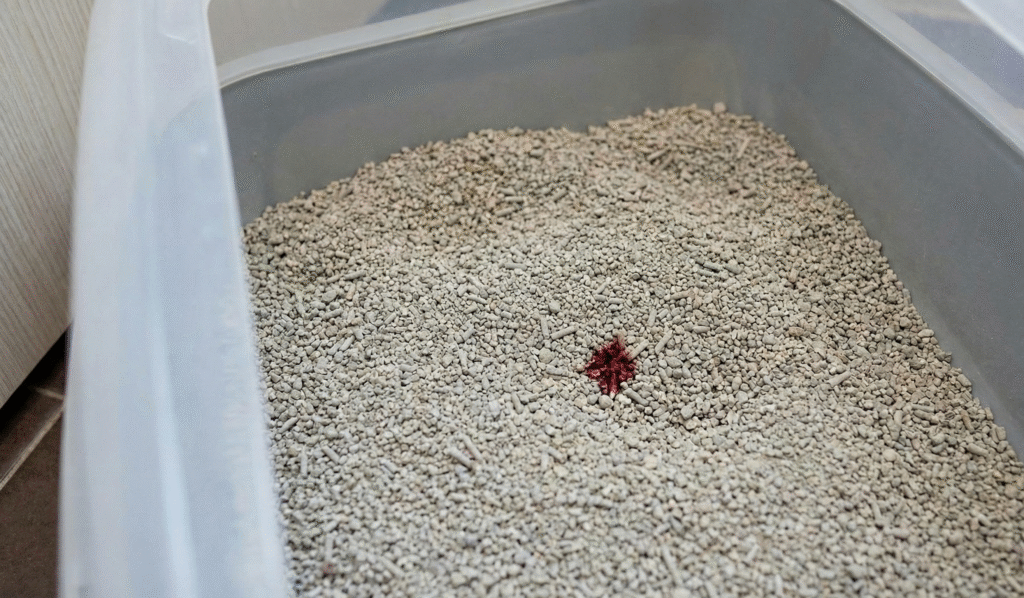
10. Urinary Issues
While urinary issues are most common with chronic kidney disease in cats, these issues can come up with kidney stones or urinary crystals as well. These problems often cause:
- Blood in the urine
- Straining or discomfort
- Frequent small urinations
- Vocalizing in the litter box
Kidney stones in cats sometimes overlap with CKD, and untreated stones can worsen kidney function.
If stones are found, kidney stones in cats treatment depends on their size and location. A veterinarian may recommend diet changes, monitoring, or medical procedures if needed. Early detection is key, which is why noticing urinary changes matters so much.
How Do Vets Diagnose Chronic Kidney Disease in Cats?
When pet owners notice early signs of chronic kidney disease in cats, the next step is a veterinary evaluation. Diagnosing kidney problems involves ruling out other conditions (like kidney stones in cats) and identifying how well the kidneys are still working.
Here’s what vets typically evaluate:
1. Full Physical Exam
A vet first checks:
- hydration
- weight and muscle condition
- mouth and gums (for ulcers or odor)
- abdominal discomfort
- heart rate and temperature
- These findings can point toward kidney stress, dehydration, or discomfort related to stones.
2. Blood Tests (Kidney Function Markers)
Two key markers help identify CKD in cats:
- Creatinine: a waste product that increases when kidneys filter less efficiently.
- BUN (Blood Urea Nitrogen): also rises when waste products accumulate.
- SDMA (Symmetric Dimethylarginine): a newer biomarker that rises earlier than creatinine, helping detect CKD sooner.
These values don’t differentiate between CKD and kidney stones in cats, but they help show how much the kidneys are affected.
3. Urinalysis
Urine tests help determine:
- concentration (dilute urine is a sign of CKD in cats)
- presence of crystals
- protein levels
- blood in the urine
4. Imaging (X-rays or Ultrasound)
- Imaging helps vets see the kidneys and check for:
- stones
- kidney size and shape
- inflammation or scarring
- blockages
- cysts or masses
5. Blood Pressure Check
High blood pressure is common in chronic kidney disease in cats and can worsen kidney damage if not detected.
CKD vs Kidney Stones in Cats — What’s the Difference?
Even though both affect the kidneys, they’re very different conditions.
- Cause
- CKD (Chronic Kidney Disease)
- Slow, long-term loss of kidney function
- Often age-related
- Can also result from infections, toxins, genetics, or previous injuries
- Progresses over months to years
- Kidney Stones in Cats
- Hard mineral buildups in the kidneys
- Often caused by mineral imbalances, dehydration, or concentrated urine
- Can be present without causing kidney failure
- May cause sudden symptoms rather than slow ones
- CKD (Chronic Kidney Disease)
- Symptoms
- CKD Symptoms
- Increased thirst
- Frequent urination
- Weight loss
- Poor appetite
- Vomiting
- Bad breath
- Dull coat
- Lethargy
- Kidney Stone Symptoms:
- Blood in urine
- Straining to urinate
- Crying in the litter box
- Abdominal discomfort
- Sometimes no symptoms at all
- Sudden pain if a stone moves
- Many owners confuse stones with urinary tract infections or CKD, which is why diagnosis matters.
- CKD Symptoms
- How They Look on Tests
- CKD:
- Elevated creatinine / BUN
- High SDMA
- Dilute urine
- Enlarged or shrunken kidneys on imaging
- Kidney Stones:
- Blood in urine
- Crystals in urinalysis
- Stones visible on X-ray or ultrasound
- Kidney values may be normal unless stones block the kidney
- CKD:
Treating Chronic Kidney Disease In Cats (CKD)
There is no cure for CKD, so treatment focuses on slowing progression and maintaining quality of life. The core pillars are:
- Dietary Modification: This is the most effective treatment of chronic kidney diseases in cats. Therapeutic renal diets are restricted in phosphorus (to slow kidney damage) and have moderate levels of high-quality protein (to reduce toxic waste). They are often calorie-dense and include omega-3 fatty acids.
- Hydration: Dehydration is a constant risk. Strategies include feeding wet food, using water fountains, and administering subcutaneous (SQ) fluids at home (injecting fluids under the loose skin of the neck/back).
- Medications:
- Phosphate Binders: If diet alone doesn’t lower phosphorus levels.
- Potassium Supplements: CKD cats often lose potassium in their urine.
- Anti-nausea/Appetite Stimulants: Medications like Cerenia (anti-nausea) or Mirataz (appetite stimulant) help keep the cat eating.
- Blood Pressure Meds: Hypertension is common in CKD cats and damages kidneys further.

Treating Kidney Stones (Nephroliths)
Note: Users often say “kidney stones” when referring to bladder stones. True kidney stones (located inside the kidney itself) are harder to treat.
- Calcium Oxalate Stones (Most Common): These cannot be dissolved with diet or medication.
- Treatment: If they are not causing a blockage, they are usually left alone and monitored via ultrasound (“benign neglect”).
- Removal: If they cause a blockage (ureteral obstruction), surgery or a bypass device (SUB – Subcutaneous Ureteral Bypass) is required.
- Struvite Stones: These are rarer in the kidney but common in the bladder. They can sometimes be dissolved with special acidifying diets, but this is risky for CKD cats (see below).
| Feature | Stone Dissolution Diet (Struvite) | Kidney Disease Diet (CKD) | The Conflict |
| Urine pH | Acidifies urine (low pH) to dissolve crystals. | Alkalinizes urine (neutral/high pH) to prevent metabolic acidosis. | Acidifying urine can make CKD in cats worse. |
| Protein | Often normal to high to acidify urine. | Restricted to reduce kidney workload. | High protein stresses the kidneys. |
| Sodium | Sometimes increased to encourage drinking. | Restricted to control blood pressure. | High sodium is bad for CKD hypertension. |
The “Multifunction” Approach
Veterinarians typically prioritize the chronic kidney disease in cats because it is life-threatening, whereas stones are often manageable.
- Use a “Renal Support” Diet with an Index: Many modern renal diets (e.g., Royal Canin Renal Support or Hill’s k/d) now carry an “S/O Index” or “S+OXSHIELD”. This means the food is formulated to create a urinary environment that prevents new stones (both struvite and calcium oxalate) from forming, even while treating the kidney disease.
Note: These diets are great for prevention but usually cannot dissolve existing large struvite stones.
- Hydration is the “Universal Cure”: Diluting the urine helps BOTH conditions. It flushes out kidney toxins and prevents minerals from clumping into stones. Feeding exclusively wet food is often the single best thing you can do.
- Surgery vs. Dissolution: If a CKD cat has a stone that must come out, veterinarians may prefer surgical removal (cystotomy) rather than trying to dissolve it with an aggressive acidifying diet, which could crash the cat’s kidney function.
Conclusion
Chronic kidney disease in cats is one of the most common conditions seen in aging felines, and early detection truly makes the biggest difference. Even though CKD can’t be reversed, noticing subtle symptoms—like increased thirst, weight loss, or changes in urination—helps owners seek veterinary care before the disease becomes advanced.
Understanding how CKD differs from issues such as kidney stones in cats also allows owners to recognize when sudden changes might mean something more urgent is happening. With proper monitoring, supportive care, hydration, and regular checkups, many cats with CKD continue to enjoy comfortable, happy lives for years.
For cat owners, the goal isn’t perfection, it’s awareness. Paying attention to early signs and partnering with a veterinarian gives cats the best chance at maintaining their quality of life, even with a chronic condition.